Rapid Sequence Intubation (RSI)

The decision to perform RSI in the ‘out of theatre’ setting involves weighing the pros and cons:
- Lack of airway protection despite patency (swallow, gag, cough, positioning , and tone)hypoxia
- hypoventilation
- need for neuroprotection (e.g. target PaCO2 35-40 mmHg)
- impending obstruction (e.g. airway burn, penetrating neck injury)
- prolonged transfer
- combativeness
- humane reasons (e.g. major trauma requiring multiple interventions)
- cervical spine injury (diaphragmatic paralysis)
- urgent need to OT and theatre is available anatomically or pathologically difficult airway (e.g. congenital deformity, laryngeal fracture)
- close proximity to OT
- paediatric cases (especially
- hostile environment
- poorly functioning team
- lack of requisite skills among team
- emergency surgical airway is not possible (e.g. neck trauma, tumour)
FACTORS THAT MAKE EMERGENCY INTUBATION DIFFICULT
RSI is useful if the following are present (from Richard Levitan’s Airwaycam.com):
- Dynamically deteriorating clinical situation, i.e., there is a real “need for speed”
- Non-cooperative patient
- Respiratory and ventilatory compromise
- Impaired oxygenation
- Full stomach (increased risk of regurgitation, vomiting, aspiration)
- Extremely short safe apnea times
- Secretions, blood, vomitus, and distorted anatomy
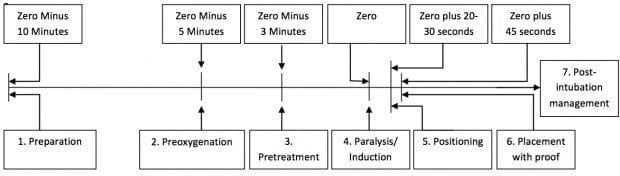
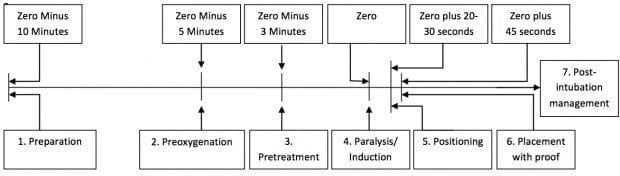
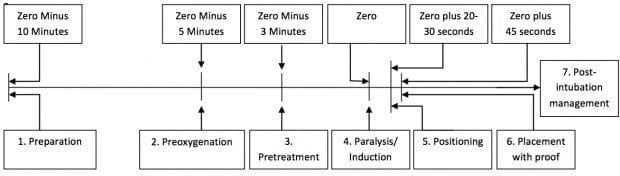
PROCESS OF RSI
Remembered as the 9Ps:
- Plan
- Preparation (drugs, equipment, people, place)
- Protect the cervical spine
- Positioning (some do this after paralysis and induction)
- Preoxygenation
- Pretreatment (optional; e.g. atropine, fentanyl and lignocaine)
- Paralysis and Induction
- Placement with proof
- Postintubation management
Some add a 10th P for (cricoid) pressure after pretreatment but this procedure is optional and has many drawbacks (see Cricoid Pressure)
Ideally, minimise instrumentation and suctioning prior to intubation to avoid stimulation of the patient’s gag reflex.
ROLES DURING RSI
The airway team should be a minimum of 3 people:
- airway proceduralist
- airway assistant
- drug administrator
The team leader may perform one of the above roles if necessary, but should ideally be a separate stand alone role.
Other roles include:
- person to perform MILS if indicated
- person to perform cricoid pressure (if deemed necessary)
- scribe
In the event of a failed airway, another person may take on the role of the airway proceduralist and role re-allocation must be clearly communicated to the team.
PREPARATION FOR RSI
Preparation requires control over:
Maintain a ‘sterile cockpit environment’ when communicating the airway plan to the team, ideally through use of a ‘call and response’ checklist— otherwise one of these two mnemonics will help:
SOAPME
- Suction
— at least one working suction, place it between mattress and bed
- Oxygen
— NRBM and BVM attached to 15 LPM of O2, preferably with nasal prongs for apneic oxygenation
- Airways
— 7.5 ET tube with stylet fits most adults, 7.0 for smaller females, 8.0 for larger males, test balloon by filling with 10 cc of air with a syringe
— Stylet – placed inside ET tube for rigidity, bend it 30 degrees starting at proximal end of cuff (i.e. straight to cuff, then 30 degree bend)
— Blade – Mac 3 or 4 for adults – curved blade
— Miller 3 or 4 for adults – straight blade
— Handle – attach blade and make sure light source works
— Backups – ALWAYS have a surgical cric kit available!
— have video laryngoscope, LMA and bougie at bedside
- Pre-oxygenate – 15 LPM NRBM
- Monitoring equipment/Medications
— Cardiac monitor, pulse ox, BP cuff opposite arm with IV
— Medications drawn up and ready to be given
- End Tidal CO2
O2 MARBLES is an alternative for the equipment and planning:
- Oxygen
- masks (NP, NRB, BVM); monitoring
- airway adjuncts (e.g. OPA, NPA, LMA); Ask for help and difficult airway trolley
- RSI drugs; Resus drugs
- BVM; Bougie
- Laryngoscopes; LMA
- ETTs; ETCO2
- Suction; State Plan
IDEAL RSI INDUCTION AGENT
Does not exist (unfortunately!), but if it did it would:
- smoothly and quickly render the patient unconscious, unresponsive and amnestic in one arm/heart/brain circulation time
- provide analgesia
- maintain stable cerebral perfusion pressure and cardiovascular haemodynamics
- be immediately reversible
- have few, if any, side effects
DRUG DOSAGES FOR RSI
Regarding doses given below:
- doses shown are for intravenous (IV) administration
- IBW = ideal body weight, TBW = total body weight
- doses may need to be adjusted in the hypotensive or shocked patient (see Intubation, Hypotension and Shock)
- Ketamine 1.5-2 mg/kg IBW
- Etomidate 0.3-0.4 mg/kg TBW
- Fentanyl 2-10 mcg/kg TBW
- Midazolam 0.1-0.3 mg/kg TBW
- Propofol 1-2.5 mg/kg IBW + (0.4 x TBW) (others simply use 1.5 mg/kg x TBW as the general guide)
- Thiopental 3-5 mg/kg TBW
- Suxamethonium 1-2 mg/kg TBW
- Rocuronium 0.6-1.2 mg/kg IBW
- Vecuronium 0.15-0.25 mg/kg IBW
INDUCTION AGENTS
- Dose: 1.5 mg/kg IV (4mg/kg IM)
- Onset: 60-90 sec
- Duration: 10-20 min
- Use: any RSI, especially if hemodynamically unstable (OK in TBI, does not increase ICP despite traditional dogma) or if reactive airways disease (causes bronchodilation)
- Drawbacks: increased secretions, caution in cardiovascular disease (hypertension, tachycardia), laryngospasm (rare), raised intra-ocular pressure
- Dose: 3-5 mg/kg IV TBW
- Onset: 30-45 sec
- Duration: 5-10 min
- Use: any RSI if haemodynamically stable, status epilepticus
- Drawbacks: histamine release, myocardial depression, vasodilation, hypotension, must NOT be injected intra-arterially due to risk of distal ischaemia, contra-indicated in porphyria
- Propofol 1-2.5 mg/kg IBW + (0.4 x TBW) (others simply use 1.5-2.5 mg/kg x TBW as the general guide)
- Onset: 15-45 seconds
- Duration: 5 – 10 minutes
- Use: Haemodynamically stable patients, reactive airways disease, status epilepticus
- Drawbacks: hypotension, myocardial depression, reduced cerebral perfusion, pain on injection, variable response, very short acting
- Dose IV 2-10 mcg/kg TBW
- Onset:
- Duration: dose dependent (30 minutes for 1-2 mcg/kg, 6h for 100 mcg/kg)
- Use: may be used in a low dose as a sympatholytic premedication (e.g. TBI, SAH, vascular emergencies); may used in a’modified’ RSI approach in low doses or titrated to effect in cardiogenic shock and other hemodynamically unstable conditions
- Drawbacks: respiratory depression, apnea, hypotension, slow onset, nausea and vomiting, muscular rigidity in high induction doses, bradycardia, tissue saturation at high doses
- Dose: 0.3mg/kg IV TBW
- Onset: 60-90 sec
- Duration: 15-30 min
- Use: not usually recommended for RSI, some practitioners use low doses of midazolam and fentanyl for RSI of shocked patients
- Drawbacks: respiratory depression, apnea, hypotension, paradoxical agitation, slow onset, variable response
- 0.3mg/kg IV
- onset: 10-15 seconds
- Use: suitable for most situations including haemodynamically unstable, other than sepsis or seizures
- Drawbacks: adrenal suppression, myoclonus, pain on injection, not available in Australia
PARALYTIC AGENTS
Suxamethonium (aka succinylcholine)
- Dose: 1.5 mg/kg IV (2 mg/kg IV if myasthenia gravis) and 4 mg/kg IM (in extremis)
- Onset: 45-60 seconds
- Duration: 6-10 minutes
- Use: widely used unless conra-indicated; ideal if need to extubate rapidly following an elective procedure or to assess neurology in an intubated pateint
- Drawbacks: numerous contra-indications (hyperkalemia, malignant hyperthermia, >5d after burns/ crush injury/ neuromuscular disorder), bradycardia (esp after repeat doses), hyperkalemia, fasciculations, elevated intra-ocular pressure, will not wear off fast enough to prevent harm in CICV situations
- Dose: 1.2 mg/kg IV IBW
- Onset: 60 seconds
- Use: can be used for any RSI unless contra-indication or require rapid recovery for extubation after elective procedure or neurological assessment; ensures persistent ideal conditions in CICV situation (i.e. immobile patient for cricothyroidotomy) – can be reversed by sugammadex
- Drawbacks: allergy (Rare)
- Dose: 0.15 mg/kg IV (may be preceded by a 0.01 mg/kg IV priming dose 3 minutes earlier)
- Osent: 120-180 econds
- Duration: 45-60 minutes
- Use: not recommended for RSI, unless no suxamethonium or rocuronium cannot be used – can be reversed by sugammadex
- Drawbacks: allergy (rare), slow onset, long duration
PRETREATMENT AGENTS
- see pretreatment drugs for RSI
RSI IN DIFFICULT SETTINGS
Ensure 360 degree access to the patient
- consider ‘scoop and run’ (e.g. from prehospital envirnoment to ED, or from ward to recovery/ ICU)
- RSI is rarely practical in the position that the patient is found, whether that be prehospital or on the ward
- airway equipment (e.g. prehospital ‘kit dump’), monitors and the airway assistant are typically on the patient’s right
RSI in an ambulance
- intubation of a patient on the ground:
- best eye line for intubator if intubator is lying prone
- prone intubator is at a mechanical disadvanatge, this can be overcome by perfroming intubatiion with the patient in the left lateral position- but this is more technically challenging and the intubator should have left elbow padding
- can place patient on spine board or equivalent and raise
- can perform with intubator kneeling (use knee pads)
RSI in aircraft
- have a low threshold for RSI prior to take off
- in aircraft there is variable access to the airway and the whole patient so intubation should be avoided if possible
- in confined space aircraft, the approach is to pre-oxyegnate and then land for RSI (PALM may be performed if needed)
- in non-confined space airacraft landing may still be the preferred option
- intubation in an aircraft may be needed in certain settings (e.g. resuce from a hostile environment)
RSI in a ward environment
- consider transfer to recovery/ ICU for RSI
- exercise crowd control
- adjust and move beds and other equipment as required
- ensure access to the patient
- consider the needs of other patients nearby
References and Links
CCC Airway Series
- Bernhard M et al. The First Shot Is Often the Best Shot: First-Pass Intubation Success in Emergency Airway Management. Anesth Analg. 2015; 121(5):1389-93. PMID 26484464
- El-Orbany M, Connolly LA. Rapid sequence induction and intubation: current controversy. Anesth Analg. 2010 May 1;110(5):1318-25. doi: 10.1213/ANE.0b013e3181d5ae47. Epub 2010 Mar 17. PMID: 20237045. [Free Full Text]
- Stept WJ, Safar P. Rapid induction-intubation for prevention of gastric-content aspiration. Anesth Analg. 1970 Jul-Aug;49(4):633-6. PMID: 5534675.
- Stewart JC, Bhananker S, Ramaiah R. Rapid-sequence intubation and cricoid pressure. Int J Crit Illn Inj Sci [serial online] 2014
FOAM and web resources
- Airwaycam.com
- ALIEM — Paucis Verbis card: Rapid Sequence Intubation
- EM Lyceum — Rapid Sequence Intubation, Episode 1 and RSI Episode 2: Induction, “Answers”
- Emergency Medicine News — The Ten Ps of Rapid Sequence Intubation by Darren Braude
Critical Care
Chris Nickson
Chris is an Intensivist and ECMO specialist at the Alfred ICU in Melbourne. He is also a Clinical Adjunct Associate Professor at Monash University. He is a co-founder of the Australia and New Zealand Clinician Educator Network (ANZCEN) and is the Lead for the ANZCEN Clinician Educator Incubator programme. He is on the Board of Directors for the Intensive Care Foundation and is a First Part Examiner for the College of Intensive Care Medicine. He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives.
After finishing his medical degree at the University of Auckland, he continued post-graduate training in New Zealand as well as Australia’s Northern Territory, Perth and Melbourne. He has completed fellowship training in both intensive care medicine and emergency medicine, as well as post-graduate training in biochemistry, clinical toxicology, clinical epidemiology, and health professional education.
He is actively involved in in using translational simulation to improve patient care and the design of processes and systems at Alfred Health. He coordinates the Alfred ICU’s education and simulation programmes and runs the unit’s education website, INTENSIVE. He created the ‘Critically Ill Airway’ course and teaches on numerous courses around the world. He is one of the founders of the FOAM movement (Free Open-Access Medical education) and is co-creator of litfl.com, the RAGE podcast, the Resuscitology course, and the SMACC conference.
His one great achievement is being the father of three amazing children.
4 Comments
Barbara Thomas
Dr. Nickson
My name is Barbara Thomas, a graduate student at Simmons University. My colleagues, Jessica, Scott, and I are working on a retrospective study considering the use of succinylcholine verses rocuronium , wich is most effective in first pass rsi in flight medicine. We are having a hard time finding new material. Most everything is dated. Any idea of where to look other than Cochran’s, and the flight sites. Thank you, I much appreciate your input. Barbara Thomas
Maurice
Fantastic Chaps
Jon
Is the midazolam dose correct? Should it be 0.03mg/kg?
James Pearlman
Hi Jon,
Yes, these are the correct dosing suggestions. 0.03mg/kg would only be 3mg in me (100kg adult) which will probably be good for some pre-op anxiolysis / anterograde amnesia for me!
In paediatrics (not my speciality, but from what I can find with my drug reference manual):
– Neonatal: Loading dose should not be used. Can use for infusion post induction
– Non-neonatal: 0.05-0.15mg/kg IV
I guess in an RSI, do you really want to use midazolam though? Is the onset of 3-5mins going to be fast enough?
Food for thought!
James
Leave a ReplyCancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed.